GI Oncosurgery
Dr. Nikhil Shellagi
MS Surgery, DNB Surgical Gastroenterology Fellowship in HPB and Liver Transplantation

Gastrointestinal Cancer Surgeon in Bangalore
GI Oncosurgery
Gastro-intestinal Oncosurgery is a subspecialty, which deals with the management of cancer of esophagus, stomach, small bowel, colon, rectum, anal canal, gall bladder & biliary tract, pancreas and liver.
- Esophagus
- Stomach
- Duodenum
- Small Intestine
- Large Intestine & Rectum
- Anal Canal
- Retroperitoneal tumours
Esophageal Cancer
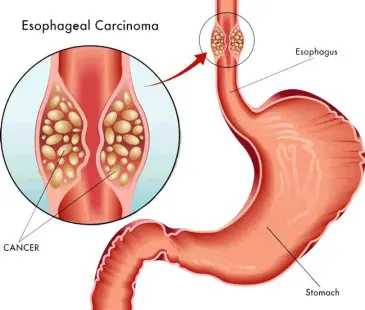
Esophageal cancer is a tumor that forms in tissue lining the esophagus. The esophagus or gullet is the muscular tube through which food passes from the throat to the stomach. The two main types of esophageal cancer are squamous cell carcinoma and adenocarcinoma. Both types occur at about the same frequency. Squamous cell carcinomas are most prevalent in Asia, whereas adenocarcinomas are more prevalent and increasing rapidly in Western countries. Most esophageal cancers occur in people older than 65. Squamous cell carcinomas are mainly associated with alcohol intake and smoking whereas adenocarcinomas are mainly associated with gastroesophageal reflux which is more related to obesity.
Risk factor for squamous cell carcinoma: Tobacco use,Alcohol consumption,Low intake of fresh fruits and vegetables,Drinking maté, Betel quid chewing, certain medical conditions e.g; Achalasia, tylosis and Plummer-Vinson syndrome.
Risk factor for Adenocarcinoma Barrett’s esophagus,Gastroesophageal reflux-disease,Obesity. Tobacco use and alcohol consumption can both increase the risk of adenocarcinoma, although the effect is smaller than in squamous cell carcinoma.
Symptoms:
• Difficulty in swallowing (dysphagia)
• hiccups, or food coming back up the esophagus
• Unexplainable weight loss
• Pain or discomfort in the throat or in the back
• Hoarseness
• Long-lasting cough
• Vomiting, or coughing up blood
Small Intestinal cancer
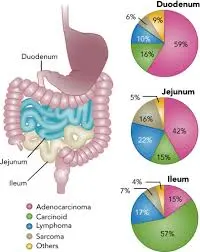
Cancer of the small bowel is rare, accounting for 1% of gastro-intestinal malignancies. Adenocarcinomas are the most common of small bowel malignancies, followed by carcinoid tumours, lymphomas, and leiomyosarcomas. Around half of all small bowel adenocarcinomas are located in the duodenum, making this the most favoured site.
Risk Factors
Sex: Small intestine cancer occurs slightly more often in men than in women.
- Age: Cancers of the small intestine tend to occur more often in older people. They are most often found in people in their 60s and 70s.
- Race/ethnicity
- Smoking and alcohol use
- Diet: Some research has suggested that diets high in red meat and salted or smoked foods might raise the risk of small intestine cancer.
- Celiac disease
- Colon cancer: People who have had colon cancer have an increased risk of getting cancer of the small intestine.
- Crohn’s disease: Crohn’s disease is a condition in which the immune system attacks the gastrointestinal (GI) tract. This disease can affect any part of the GI tract, but it most often affects the lower part of the small intestine. People with this condition have a much higher risk of small intestine cancer (particularly adenocarcinoma).
- Inherited syndromes: People with certain inherited conditions have a higher risk of small intestine cancer (mainly adenocarcinoma).
- Familial adenomatous polyposis (FAP)
- Lynch syndrome (hereditary nonpolyposis colorectal cancer, or HNPCC)
- Peutz-Jeghers syndrome (PJS)
- Cystic fibrosis (CF): People with CF have an increased risk of small intestine cancer
Symptoms:
- Blood in the stool (feces)
- Dark/black stools
- Diarrhea
- A lump in the abdomen
- Pain or cramps in the abdomen
- Unexplained weight loss
Diagnosis
Routine blood investigations
Contrast Enhanced CT Scan of abdomen wold help us to stage the disease It should be pointed out that in a context of obscure bleeding after upper and lower endoscopy, a small bowel investigation should systematically be done. New investigation tools, such as CT enteroclysis, MR enteroclysis, capsule endoscopy now allow for an extensive exploration of small bowel and should thus make early diagnosis possible. Diagnosis Routine blood investigations Contrast Enhanced CT Scan of abdomen wold help us to stage the disease It should be pointed out that in a context of obscure bleeding after upper and lower endoscopy, a small bowel investigation should systematically be done. New investigation tools, such as CT enteroclysis, MR enteroclysis, capsule endoscopy now allow for an extensive exploration of small bowel and should thus make early diagnosis possible.
Treatment
Complete resection (R0) of the primary tumour with loco-regional lymph node resection is mandatory. In the context of posterior invasion, pre-operative treatment should be considered, and resection reconsidered after 2–3 months of chemotherapy. In the context of unresectable metastases, primary tumour resection is not recommended except in an emergency such as bowel obstruction, perforation or uncontrolled bleeding. For duodenal tumours, a Whipple resection should be performed for a tumour in the second segment of the duodenum or for an infiltrating tumour in the proximal or distal duodenum. A duodenal resection alone could be performed for a proximal duodenal tumour or a distal duodenal tumour with no infiltration of adjacent organs. For jejunal and ileal tumours, an R0 resection with lymph node resection and jejuno-jejunal or ileo-ileal anastomosis should be performed. For atumour in distal ilal segment, an ileocoecal or right hemicolectomy should be performed with ligation of the ileocolic artery so as to allow for lymph node resection.
Colorectal cancer
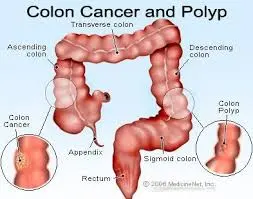

Colon cancer refers to cancer that develops in the colon, the longest part of the large intestine. Rectal cancer develops in the rectum, the final straight part of the large intestine that ends in the anus.
Risk factors:
- Aging: the risk of colorectal cancer increases as a person gets older.
- Lifestyle-related risk factors
- Diet: diet is the most important environmental risk factor for colorectal cancer. A diet that is high in red meat and processed meat, high in fat and/or low in fiber can increase the risk of developing colorectal cance
- High consumption of alcohol
- Obesity: overweight increases the risk of developing colorectal cancer
- Sedentary lifestyle
- Smoking
- Diabetes mellitus type 2 increases the risk of developing a tumour in the large intestine.
- Previous history of colorectal polyps
- Previous history of colorectal cancer
- Inflammatory bowel disease such as Crohn’s disease or ulcerative colitis
- Family history: approximately 20 % of colorectal cancers occur in a familial context
Symptoms
change in bowel habits, abdominal discomfort, fatigue, weight loss.Blood in stools could be a sign of alert. It could be visible to the naked eye or through a laboratory analysis of stools.
Investigations:
Colonoscopy
lighted tube is inserted through the anus into the intestine. It allows seeing the inside of the intestine. When a tumour is found within 15 cm from the anus it is considered rectal tumour, further away it is considered colon tumour.
CECT Abdomen and Pelvis for staging of disease
MRI Pelvis for staging of rectal cancer
PET CT in Advanced colorectal cancer
Tumour markers:CEA
Surgery
Surgery is the most usual treatment for colon cancer, especially if it has not developed. As for many cancers, surgery for colon cancer is most successful when done by a surgeon with a great deal of knowledge in the procedure.
Laparoscopic surgery
Laparoscopic surgery The word “laparoscopy” means to look inside the abdominal hole with a special camera or scope. To do a laparoscopy, between 3 and 6 small (5-10 mm) cuts are made in the stomach. The laparoscope and special laparoscopic tools are entered through these small holes. The surgeon is then guided by the laparoscope, which gives a picture of the intestinal organs on a video monitor.
Polypectomy
A colonoscopy, which is a large tube with a camera on the end, is entered into the rectum and guided to the polyp. A tiny, scissor-like device or wire loop removes the polyp.
Colectomy
The region of the colon where the cancer is, along with some healthy surrounding muscle, is removed. The associated lymph nodes are removed and looked at under a scope. Usually, the doctor then rejoins the sections of the colon. This operation also is called a hemicolectomy or partial colectomy.
Chemotherapy
Prolife offers the most up-to-date and effective chemotherapy choices for Colon cancer. Drugs are given by mouth or intravenously
Targeted therapy
Targeted therapy targets cancer’s specific genes, proteins, or the tissue conditions that add to cancer growth and survival. Targeted therapy blocks the increase and spread of cancer cells while restricting the damage to normal cells.
Radiation therapy
Radiation therapy uses strong energy sources, such as X-rays and protons, to kill cancer cells. It might be used to withdraw large cancer before an operation so that it can be removed more quickly.
When surgery isn’t an option, radiation therapy might be used to reduce signs, such as pain. Sometimes radiation is mixed with chemotherapy.
Anal Cancer
The anal canal is defined as the terminal part of the large intestine, beginning at the upper surface of the anorectal ring and passing through the pelvic floor to end at the anus.
The most frequent neoplams of this region are HPV-associated squamous cell carcinomas (SCC) and adenocarcinomas.
In most settings, SCC compromises more than 70% of cases. In the general population, anal cancer is uncommon, with age-standardized incidence rates mostly between 1 and 2 per 100000 per year. However, the incidence of anal SCC is increasing by 1-3% per year in developed country settings. High-risk HPV types can be detected in 80-90% of all anal SCC cases, making it second only to cervical cancer in the closeness of its association with this virus.
The Risk Factors
- HPV infection with high risk genotypes
- Cervical dysplasia, cervical cancer, or genital warts
- HIV seropositivity and low CD 4 count
- Cigarette smoking
- Anoreceptive intercourse
- Immune suppresion following transplant (100x increase in KTX)
Clinical Presentation
- Rectal bleeding- 45% of patients
- Pain or sensation of mass- 30%
- No symptoms- 20%
- Pruritus ani or bleeding plaques associated with anal margin skin cancers- Paget’s disease
The diagnostic Workup
- Physical exam- rectal and nodes
- Biopsy- used to differentiate squamous cell (anal ca) from adenocarcinoma (rectal ca) does not have to be excisional
- CT scan to evaluate for metastatic disease
- EUS to evaluate for sphincter involvement and perianal lymph nodes
- PET scan since 25% of patients have metastatic disease by PET not seen on CT and 20% of inguinal nodes negative by CT are PET positive.
Treatment
Planning of the treatment involves an inter-disciplinary team of medical professionals.
The treatment will usually combine intervention methods that:
- Act on the cancer locally, such as surgery or radiotherapy
- Act on cancer cells all over the body by systemic therapy such as chemotherapy
Surgery:
The main goal of treatment is to obtain a cure with locoregional control, concomitant with the preservation of anal sphincter function and maintaining the best possible quality of life.
Squamous cell Carcinoma:
SCC represents the majority of anal canal tumors (85%). Initially, up to the 1980s surgery was the treatment for all anal carcinomas, mainly with abdominoperineal resection (APR) with 5 years survival rates achieved for 38-71% of patients and recurrence developing is 27-43%.
But now,the standard treatment for non-metastatic squamous cell carcinoma of the anal canal has been a combination therapy, with chemotherapy and radiotherapy with a radiation providing a complete regression in 80–90% of patients. Approximately, 15% of patients will have persistent disease initially while a further 15% will develop late locoregional recurrence. The 5 years survival figures of 60-80%, along with an 80% preservation of anal function, makes non-surgical management an attractive option for anal canal tumors.
Surgery
(abdominoperineal resection and permanent colostomy) in SCC is reserved for patients with residual or recurrent disease after a complete treatment of chemo radiotherapy.
Surgery after recurrence allows a local control in 60% of cases and a survival at 5 years of 30–60%
Adenocarcinoma :
Adenocarcinoma of the anal canal are rare tumors (15%) and are thought to arise in the ducts or the intramuscular anal glands, and in the long-standing fistulas. These neoplasm affect older age groups and have no sexual predominance. Most of these lesions are slow growing, locally aggressive, and rarely metastasize. The abundant mucin production of these tumors may explain their tendency to dissect soft tissue planes. A wide local excision may be performed for small and well-differentiated carcinomas that have not invaded sphincter mechanism. Otherwise, APR is indicated.
Melanoma :
The anal canal is the third most common site of melanoma, exceeded only by the skin and the eyes, representing 0.3-1.6% of all melanomas. The mean age of occurrence is in the fifth decade, and females are affected more frequently than males. Surgery provides the only hope for cure, but significance differences in survival between patients treated with local excision and those with APR have not been demonstrated. However, APR seems to provide better local control of the disease. Unfortunately, local recurrence in these cases was often accompanied by the appearance of distal or regional metastases as well. Radio-chemotherapy has demonstrated little benefit in this disease. Patients treated in a curative fashion have a survival of 6-20%.
Treatment of Locally Recurrent and Metastatic Disease with Chemotherapy:
Different regimens of salvage chemotherapy may be used for metastatic anal carcinoma, although the most common regimens at present employ Cisplatin and 5-FU.4