Gastrointestinal Surgery
Dr. Nikhil Shellagi
MS Surgery, DNB Surgical Gastroenterology Fellowship in HPB and Liver Transplantation

Best Gastrointestinal Surgery in Bangalore
Gastrointestinal Surgery
Various surgical procedures are used in gastrointestinal surgery to identify and treat GI disorders. Depending on the issue or condition, surgery can be performed on both the upper and lower GI tracts.
- Cholecystectomy
- Appendicectomy
- Splenectomy
- Hiatus hernia, achalasia Cardia
- Repair of inguinal and ventral hernias in the abdomen
- Strictures, inflammatory bowel disease, intestinal perforation, and peptic ulcer surgery
- Corrosive esophageal stricture surgery

GERD (Gastroesophageal Reflux Disease)
The disordered valve mechanism between the oesophagus (swallowing tube) and the stomach causes the acidic and secretory contents of the stomach to flow back into the oesophagus, causing gastroesophageal reflux disease (GERD).
The esophageal lining may become damaged due to the food, acids, and digestive enzymes flowing backward (reflux).
- Heartburn: A burning sensation in the centre of the chest behind the breastbone, which has an upward moving quality toward the throat.
- Acid regurgitation: The awareness of acid or partially digested food from the stomach backing up into the esophagus, and occasionally into the throat and mouth.
- Other GERD symptoms may include:
- Difficulty swallowing
- Excessive burping or belching
- Sour or bitter taste in the mouth
- Chest pain
- Abdominal pain
- Nausea or gagging
- Cough, sore throat or hoarseness
- Obesity
- Pregnancy
- Hiatus hernia
- Food choices
- Smoking
- Family history of GERD
Endoscopy: A thin, flexible tube (endoscope) with a light and a tiny camera is inserted into the oesophagus for this safe test.
Barium X-ray (upper GI series): The lining of the upper digestive tract is coated with barium so that it can be seen on an X-ray. 24-hour pH monitoring: In the oesophagus is a tiny tube (catheter) that has a pH sensor on it.
Over the course of a day, the sensor measures how acidic the oesophagus is, and the information is stored on a small computer that is worn around the waist for analysis in the future.
Esophageal motility study (EMS): In the oesophagus, a tiny tube (catheter) with a sensor is placed. The sensor used in this test gauges pressure and movement in the stomach and oesophagus to determine how well the LES is working.
- Avoid coffee, alcohol, fried or fatty foods, chocolate, peppermint, and other foods.
- Eat small, frequent meals as opposed to large ones.
- Before going to bed, wait three to four hours without eating or drinking anything.
- Using a foam wedge, raise the bed’s head or your upper body.
- attain and maintain a healthy weight
- Avoid smoking.
Medication
- Histamine H2-RAs, or H2-receptor antagonists, lessen the production of stomach acid.
- Stomach acid production is inhibited by proton pump inhibitors (PPIs). In addition to healing esophageal damage, this lessens heartburn symptoms.
- Agents that promote motility or prokinetics speed up the stomach’s emptying.
Indications for surgery include
- Ineffective medical management
- failure by the patient to comply
- excessive reflux,
- Endoscopy revealed severe esophagitis
- benign stricture resulting from ulcers or erosions
- the columnar-lined epithelium of Barrett (without severe dysplasia or carcinoma)
- being young and/or
- Patient decisions take into account the negative effects of ongoing medical treatment
Since GERD is a chronic condition, treatment must typically be continued long-term even after symptoms have been managed. Untreated GERD may occasionally cause significant esophageal damage.
Chronic scarring can cause the oesophagus to narrow (stricture), and repeated exposure to stomach acid can lead to the development of an esophageal ulcer and bleeding.
Barrett’s oesophagus, a condition that causes changes to the esophageal lining and raises the risk of esophageal cancer, may be present in some patients with long-term, uncontrolled GERD.
Since GERD is a chronic condition, treatment must typically be continued long-term even after symptoms have been managed. Untreated GERD may occasionally cause significant esophageal damage.
Chronic scarring can cause the oesophagus to narrow (stricture), and repeated exposure to stomach acid can lead to the development of an esophageal ulcer and bleeding.
Barrett’s oesophagus, a condition that causes changes to the esophageal lining and raises the risk of esophageal cancer, may be present in some patients with long-term, uncontrolled GERD.
Alarming symptoms are out of the ordinary for GERD and can point to more serious health issues.
Consult a doctor if you notice a change in your current symptoms or experience any of the following:
- Sudden weight loss
- Difficulty swallowing or a feeling that food is trapped in the chest
- Nausea / Vomiting
- Bloody stools (tarry black or red)
- Anemia

Hiatal Hernia
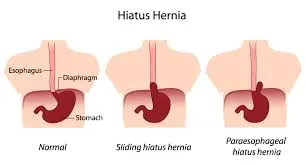
The diaphragmatic hiatus allows the esophagus to enter the abdomen. Because the hiatus is directly impacted by pressure stress between the abdomen and the chest, it is susceptible to visceral herniation.
A hiatus hernia is a condition in which the stomach is the most common abdominal organ to herniate into the mediastinum through the diaphragmatic hiatus.
Type I
The sliding hiatal hernia is the most prevalent type of hernia (95%) where the gastroesophageal junction migrates above the diaphragm. The fundus continues to be below the gastroesophageal junction, and the stomach continues to be in its normal position.
Type II
Pure para-esophageal hernias (PEH) are hernias in which a portion of the fundus pushes through the diaphragmatic hiatus next to the oesophagus while the gastroesophageal junction remains in its normal position.
Type III
Combining Types I and II, hernias happen when the gastroesophageal junction and the fundus push through the hiatus. Overlooking the gastroesophageal junction is the fundus.
Type IV
A structure other than the stomach, such as the omentum, colon, or small bowel, is present within the hernia sac, which is what distinguishes hiatal hernias from other types.
Small hernias — The majority of small hiatal hernias are problems.
Large hernias — When stomach acids back up into your oesophagus, larger hernias may result in the following signs and symptoms.
- Heartburn\s
- Belching
- Chest pain
- Nausea
When you lean forward, strain, lift heavy objects, or lie down, these signs and symptoms tend to get worse. They can also get worse during pregnancy.
Rarely, the portion of your stomach that protrudes into your chest cavity may twist (become strangulated) or lose blood, which can cause:
- Bad chest pain
- Having trouble swallowing (dysphagia)
- Having your esophagus blocked
- 50 or older
- overweight
- and smoking
Children’s paraesophageal hernias are most frequently caused by congenital defects, which are occasionally combined with other birth defects.
Endoscopy is used to diagnose the upper gastrointestinal tract when certain clinical conditions exist.
alarm signs (dysphagia, bleeding, weight loss, anaemia) or symptoms in patients older than 50 years that are typical of GERD but resistant to treatment.
Radiologic imaging: Although radiology of the upper gastrointestinal tract has a low sensitivity for mucosal complications, hiatus hernia can be diagnosed by this method. Usually, the presurgical evaluation includes a referral to radiology.
- Bleeding and anemia
- Reduced blood flow to stomach
- GERD
- Difficulty swallowing
- Barrett’s esophagus
- Esophageal Cancer
Dietary and Lifestyle Adjustments
- Avoid fried or fatty foods, chocolate, peppermint, coffee, and alcohol.
- Rather than skipping meals, eat small, frequent meals.
- For three to four hours prior to going to bed, eat nothing and drink very little to nothing.
- Use a foam wedge to raise your upper body or the head of your bed.
- Obtain and keep a healthy weight.
- Quit smoking.
Achalasia Cardia
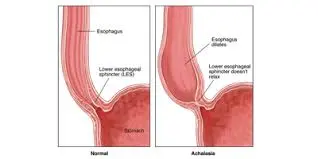
The cause of achalasia, an oesophageal motility disorder, is unknown. Achalasia causes the lower oesophageal sphincter to lose its ability to function and causes myenteric nerve plexus degeneration in the oesophageal wall.
- Progressively having trouble swallowing solids and liquids (dysphagia)
- Unabsorbed food being regurgitated Reflux
- Pneumonia from aspiration
- Loss of weight (late finding)
- Chest pain (atypical finding)
A patient with dysphagia to both solids and liquids and associated regurgitation of undigested food is typically suspected to have achalasia.
The following diagnostic techniques are frequently used in achalasia.
Endoscopy
Esophagogastroduodenoscopy (EGD) is usually necessary for patients who present with dysphagia in order to rule out a mechanical obstruction caused by cancer, which can mimic achalasia both clinically and manometrically.
Esophageal barium scan
The classic description of achalasia on a barium esophagram is esophageal dilation with a gradual taper down to the gastroesophageal junction giving a “bird’s beak” appearance. The objective measurement of esophageal emptying is the timed barium esophagogram (TBE).
Esophageal Manometry
It is the de facto method for achalasia diagnosis. Its purpose is to measure the pressures inside the esophageal along a flexible catheter’s length. Pressure data can be plotted as esophageal topography using high-resolution manometry.
Endoluminal Functional Lumen Imaging Probe (EndoFLIP)
EndoFLIP allows for the real-time measurement of gastroesophageal junction (GEJ) distensibility and operates on the impedance planimetry principle. The effectiveness of the treatment could be assessed using this parameter rather than LES pressure.
It cannot be cured but can be managed. There are five main types of treatment.
Pharmacotherapy
The least effective form of treatment for achalasia is thought to be oral pharmaceutical therapies. These drugs have an unfavourable side effect profile and a transient clinical response. The two drugs that are most frequently used are long-acting nitrates and calcium channel blockers.
Botox Injections
For patients who are unable to tolerate more invasive therapies like pneumatic dilatation or surgical myotomy, botulinum toxin is a helpful treatment option. The procedure entails evenly distributing up to 100 units of toxin with a sclero-needle just proximal to the squamo-columnar junction. The response rate is high during the first month of treatment, ranging from 80% to 90%, but the therapeutic effect quickly wears off over time, with only 50% of patients still experiencing symptoms after a year. Repeat treatments are therefore frequently needed every 6 to 12 months.
Pneumatic Dilation (PD)
The most successful non-operative treatment: 55-70% with a single dilation; >90% with multiple.
This causes the LES muscle fibres to be stretched and torn.
Most people need to receive treatment again after one dilation.
The rate of perforation is 1% (0.67–5.6%), and the overall complication rate is 11%. (Perforation, GERD, intramural hematoma).
Surgical myotomy, a procedure that divides the LES’s circular muscle fibres, was first carried out through an open thoracotomy and laparotomy.
But over time, less invasive procedures began to replace the outdated open approach. First, thoracoscopy was used instead of laparoscopic heller myotomy (LHM) due to its reduced morbidity and quicker recovery. LHM is now recognised as the gold standard for the surgical management of AC.
Esophagectomy
Conventional achalasia treatments frequently fail to control “end-stage” achalasia, which is characterised by a dilated and tortuous oesophagus (megaesophagus or sigmoid oesophagus). Before considering the more morbid esophagectomy, surgical myotomy should still be considered as the initial treatment even though PD is ineffective.
Peroral endoscopic myotomy: (POEM) is a cutting-edge endoscopic technique that myotomizes the LES using the oral cavity as a natural orifice entry point. By cutting only the inner, circular LES muscles through a submucosal tunnel made in the proximal esophageal mucosa, a surgeon performs the myotomy after tunnelling an endoscope down the oesophagus toward the esophageal gastric junction.
In contrast to laparoscopic surgery, which necessitates complete severance of the circular and longitudinal LES muscle layers, POEM does not involve this. To make it easier for food to enter the stomach, the dysfunctional muscle fibres that stop the LES from the opening are cut.